Feeling bloated after meals? Struggling with energy crashes mid-afternoon? Noticing your skin acting up no matter what products you try? These could be signs your gut needs support. As a nutritional scientist specialising in women's health, I see these patterns every day among women who come to HerNutrea seeking answers. The truth is, your gut …
Feeling bloated after meals? Struggling with energy crashes mid-afternoon? Noticing your skin acting up no matter what products you try? These could be signs your gut needs support. As a nutritional scientist specialising in women’s health, I see these patterns every day among women who come to HerNutrea seeking answers. The truth is, your gut microbiome, the trillions of bacteria living in your digestive system, affects far more than just digestion. It influences your mood, energy levels, immune function, skin health, and even your weight. In this guide, you’ll discover 10 signs your gut needs support, what each sign means, and actionable first steps you can take today to start feeling better.
 “Persistent bloating is one of the most common signs of gut microbiome imbalance”
“Persistent bloating is one of the most common signs of gut microbiome imbalance”
Table of Contents
10 Signs Your Gut Needs Support
Your body is constantly communicating with you, and your gut is one of the most vocal messengers. Here are 10 signs that shouldn’t be ignored:
1. Persistent Bloating (Especially After Meals)
What it means: If you regularly feel like you need to unbutton your jeans after eating, you’re experiencing more than just “eating too much.” Persistent bloating often indicates gas production from bacterial fermentation, possible dysbiosis (microbial imbalance), or even SIBO (small intestinal bacterial overgrowth). According to research published in Gastroenterology, bloating affects up to 30% of the general population and is often linked to gut microbiome imbalances.
When to worry: Occasional bloating after a large meal is normal. Daily bloating, especially if it worsens throughout the day or is accompanied by pain, deserves attention.
Quick tip: Keep a food-symptom diary for one week. Note what you eat, when you eat it, and how you feel 1-2 hours later. This simple practice can reveal patterns and trigger foods. You might discover that certain high-FODMAP foods like onions, garlic, or legumes are contributing to your symptoms.
2. Irregular Bowel Movements
What’s “normal”: Despite what you might think, there’s actually a wide range of “normal” when it comes to bowel movements—anywhere from three times per day to three times per week can be healthy, depending on your individual physiology.
Red flags: Chronic constipation (fewer than three bowel movements per week), chronic diarrhoea, or alternating between the two are signs your gut needs support. These patterns often indicate imbalances in gut bacteria, inadequate fibre intake, or underlying conditions such as IBS.
Quick tip: Increase your fibre intake gradually; aim for 25-30 grams daily from whole-food sources like vegetables, fruits, legumes, and whole grains. Pair this with adequate hydration (at least eight glasses of water daily). Sudden fibre increases without enough water can actually worsen constipation, so go slowly.
3. Constant Sugar Cravings
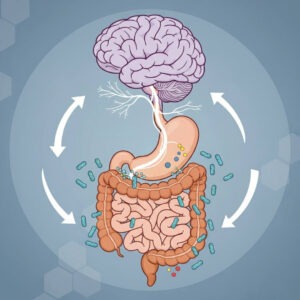
The connection: This might surprise you, but your sugar cravings aren’t just about willpower. Certain gut bacteria actually thrive on sugar and can send craving signals to your brain through the gut-brain axis. Research on the microbiome-gut-brain axis suggests that gut microbes can influence eating behaviour and mood via neural pathways.
What it means: Persistent, intense sugar cravings often indicate an imbalance in your gut flora, with sugar-loving bacteria dominating your microbiome.
Quick tip: Add fermented foods like sauerkraut, kimchi, kefir, or yoghurt to your daily diet. Studies show that introducing beneficial bacteria through fermented foods can help reduce sugar cravings over 2-4 weeks as your microbiome rebalances. Start with small amounts (1-2 tablespoons) and gradually increase.
4. Unexplained Fatigue
The gut-energy connection: Here’s a fascinating fact: approximately 90% of your body’s serotonin—a neurotransmitter crucial for mood and energy—is actually produced in your gut, not your brain. When your gut health is compromised, serotonin production can suffer, leading to fatigue, low mood, and poor sleep quality.
What it means: Persistent tiredness despite adequate sleep often points to poor nutrient absorption, chronic low-grade inflammation, or microbiome imbalances affecting neurotransmitter production.
Quick tip: Consider having your vitamin B12, iron, and vitamin D levels checked, as deficiencies in these nutrients are common with poor gut health and directly impact energy levels. Meanwhile, focus on eating nutrient-dense foods and consider adding a high-quality probiotic to support gut barrier function.
5. Skin Issues (Acne, Eczema, Rosacea)
The gut-skin axis: Your skin is often a mirror of your gut health. When your gut lining becomes inflamed or permeable (often called “leaky gut”), inflammatory compounds can travel through your bloodstream and manifest as skin problems. Research in the Journal of Clinical and Aesthetic Dermatology has established clear connections between gut health and skin conditions.
What it means: Persistent acne, eczema, rosacea, or other inflammatory skin conditions may indicate gut inflammation, dysbiosis, or food sensitivities that are triggering immune responses.
Quick tip: Try eliminating dairy for 2-3 weeks and observe any changes in your skin. Dairy is one of the most common food triggers for skin issues. Also, focus on anti-inflammatory foods rich in omega-3 fatty acids, such as wild salmon, walnuts, and flaxseeds.
6. Food Intolerances That Seem to Multiply
Why it happens: If you’ve noticed that you’re suddenly reacting to foods you used to tolerate well, your gut lining may be compromised. When the tight junctions in your intestinal wall become loose (increased intestinal permeability), partially digested food particles can pass through into your bloodstream, triggering immune reactions.
What it means: Multiple or increasing food intolerances often suggest increased intestinal permeability or significant dysbiosis that’s affecting your digestive enzyme production.
Quick tip: Focus on gut-healing foods that support the intestinal lining: bone broth (rich in collagen and glutamine), collagen peptides, omega-3 fatty acids, and zinc-rich foods like pumpkin seeds. Also consider working with a nutritionist to identify trigger foods through an elimination protocol.
7. Mood Swings, Anxiety, or Brain Fog
 “The gut-brain axis: Your microbiome directly influences mood, anxiety, and cognitive function”
“The gut-brain axis: Your microbiome directly influences mood, anxiety, and cognitive function”
The gut-brain axis: Your gut and brain are in constant communication through the vagus nerve, hormones, and immune system signalling. This bidirectional communication highway, known as the gut-brain axis, means that what happens in your gut directly affects your mental state. Studies published in Physiological Reviews demonstrate how gut microbiota influence brain function and behaviour.
What it means: Mood swings, persistent anxiety, depression, or brain fog can indicate microbiome imbalances affecting neurotransmitter production, particularly serotonin, dopamine, and GABA.
Quick tip: Incorporate probiotic-rich foods into your daily routine. Research shows that certain probiotic strains (particularly Lactobacillus and Bifidobacterium species) can improve mood and reduce anxiety symptoms within 4-6 weeks. Fermented foods like yoghurt, kefir, and sauerkraut are excellent sources. Learn more about how gut health affects hormones and mood.
8. Frequent Colds or Infections
The immune connection: Did you know that approximately 70% of your immune system resides in your gut? Your gut-associated lymphoid tissue (GALT) is your body’s largest immune organ. When your gut microbiome is imbalanced, your immune function suffers.
What it means: If you’re catching every cold that goes around or dealing with frequent infections, your gut barrier may be weakened, compromising your immune defences.
Quick tip: Feed your beneficial bacteria with prebiotic foods—these are the fibres that your good bacteria feast on. Excellent sources include garlic, onions, leeks, asparagus, bananas, oats, and Jerusalem artichokes. Aim for a variety of prebiotic foods each day to support a diverse range of beneficial bacteria.
9. Bad Breath That Won’t Go Away
Beyond dental health: While poor oral hygiene is the most common cause of bad breath, persistent halitosis despite good dental care can indicate SIBO (small intestinal bacterial overgrowth) or dysbiosis. When bacteria overgrow in the small intestine or when harmful bacteria dominate your gut, they can produce sulfur compounds that contribute to bad breath.
What it means: Chronic bad breath unrelated to dental issues may signal bacterial overgrowth in your small intestine or significant imbalances in your oral and gut microbiomes.
Quick tip: First, rule out dental issues with your dentist. If your oral health is good but bad breath persists, consider gut microbiome testing to identify potential SIBO or dysbiosis patterns. In the meantime, avoid sugar and refined carbohydrates that feed problematic bacteria.
10. Weight Changes Without Diet Changes
The microbiome-metabolism link: Your gut bacteria play a surprising role in how many calories you extract from food and how efficiently you metabolise nutrients. Research has identified that the ratio of two major bacterial groups, Firmicutes and Bacteroidetes, can influence weight management. Studies in Nature have shown that obese individuals tend to have distinct microbiome compositions compared with lean individuals.
What it means: Unexplained weight gain or difficulty losing weight despite healthy eating may indicate that your microbiome composition is affecting your metabolism and calorie extraction.
Quick tip: Focus on increasing the diversity of plant foods in your diet. Research suggests that people who eat 30+ different types of plant foods per week have more diverse, healthier microbiomes. This diversity is associated with better metabolic health and easier weight management.
What These Signs Mean for Your Health
If you’re experiencing several of these signs, it’s important to understand that they’re not just minor annoyances—they’re your body’s way of communicating that something needs attention. The good news? Gut health is highly modifiable with the right approach.
Unlike genetics, which you can’t change, your gut microbiome is dynamic and responsive to your diet, lifestyle, and environment. Small, consistent changes can lead to significant improvements in how you feel within weeks to months.
However, it’s also important to recognise that everyone’s gut microbiome is unique. What works for one person may not work for another, which is why personalised approaches based on your specific microbiome composition can be so valuable. This is where gut microbiome testing can provide insights tailored to your individual needs.
Your Next Steps
If you recognise yourself in several of these signs, here’s a practical action plan to start supporting your gut health today:
Step 1: Track Your Symptoms for 1-2 Weeks
Start a simple symptom diary. Each day, note:
- What you ate and when
- Digestive symptoms (bloating, gas, bowel movements)
- Energy levels throughout the day
- Mood and mental clarity
- Sleep quality
- Any skin changes
This tracking will help you identify patterns and potential trigger foods. You might be surprised by what you discover.
Step 2: Implement Foundational Gut-Health Practices
 “A diverse diet with 30+ plant foods per week supports a healthy, diverse microbiome”
“A diverse diet with 30+ plant foods per week supports a healthy, diverse microbiome”
These evidence-based strategies support gut health for most people:
- Eat 30+ different plant foods per week: This isn’t as hard as it sounds! Count all vegetables, fruits, whole grains, legumes, nuts, seeds, and herbs. Variety feeds diverse beneficial bacteria.
- Include fermented foods daily: Start with small amounts (1-2 tablespoons) of sauerkraut, kimchi, kefir, yogurt, or kombucha. Gradually increase as tolerated.
- Manage stress: Chronic stress directly damages your gut lining and alters your microbiome composition. Practice daily stress-reduction techniques like deep breathing, meditation, yoga, or nature walks.
- Prioritise 7-8 hours of quality sleep: Poor sleep disrupts your gut microbiome and increases intestinal permeability. Establish a consistent sleep schedule and create a relaxing bedtime routine.
- Stay hydrated: Adequate water intake supports the mucosal lining of your intestines and helps beneficial bacteria thrive.
Step 3: Consider Professional Support If Symptoms Persist
If you’ve implemented these foundational practices for 4-6 weeks and aren’t seeing improvement, it may be time to seek personalised nutrition guidance. At HerNutrea, we combine comprehensive microbiome testing with one-on-one nutritional support to create tailored strategies for your unique situation.
When to Seek Professional Help
While many gut health issues can improve with dietary and lifestyle changes, certain situations warrant professional evaluation:
- Persistent symptoms beyond 4-6 weeks despite implementing gut-supportive practices
- Severe symptoms that significantly affect your quality of life or daily functioning
- Multiple signs appearing together, especially if they’re worsening over time
- Previous diagnosis of IBS, SIBO, IBD, or other digestive conditions
- Unexplained weight loss, blood in stool, or severe abdominal pain (seek medical attention promptly)
A comprehensive approach that includes medical evaluation, gut microbiome testing, and personalised nutrition guidance can help you get to the root cause of your symptoms rather than just managing them.
Conclusion
Your gut is constantly communicating with you through these 10 signs, and they’re worth listening to. Persistent bloating, irregular bowel movements, sugar cravings, fatigue, skin issues, food intolerances, mood changes, frequent infections, bad breath, and unexplained weight changes are all signals that your gut microbiome needs support.
The empowering truth is that small, consistent changes can make big differences in how you feel. By tracking your symptoms, implementing foundational gut-health practices, and seeking personalised support when needed, you can transform your gut health and, by extension, your overall wellness.
Want deeper insights into your unique gut health? Our at-home microbiome test analyses 15+ key biomarkers to give you a personalised roadmap for optimal gut health. Discover which foods, supplements, and lifestyle changes will work best for your unique microbiome. Learn more about microbiome testing and take the first step toward feeling your best.
Ready to transform your gut health? Join our newsletter for evidence-based gut health tips, recipes, and exclusive insights delivered to your inbox weekly.